A study that showed that margarine and vegetable oils are more likely to kill you than butter was buried in the 1970s
The Minnesota Coronary Experiment found evidence that switching from saturated to unsaturated fat in vegetable oils in 1973 caused more deaths but the results were not published and we've been lied to for over 50 years.

We've been lied to about the dangers of saturated fat for over 50 years. Ancel Keys was a major contributor to the saturated fat narrative since the 1950s, when increasing cases of cardiovascular disease made it an increasingly political issue. This resulted in the standard dietary advice that people should avoid saturated fat in order to reduce their risk of developing the disease. This is a very difficult task when dealing with type 2 diabetes because reducing both saturated fat and carbohydrates will leave you feeling hungry.
The diet-heart hypothesis is the idea that dietary saturated fat increases blood cholesterol levels and this causes atherosclerosis - the build up of plaques in arterial blood vessels that ultimately lead to heart attacks and strokes. The problem with this theory is that its simplicity has led to it being assumed to be true. It has never been proven to be correct in a randomised controlled trial and yet it is still espoused by the vast majority of medical professionals.
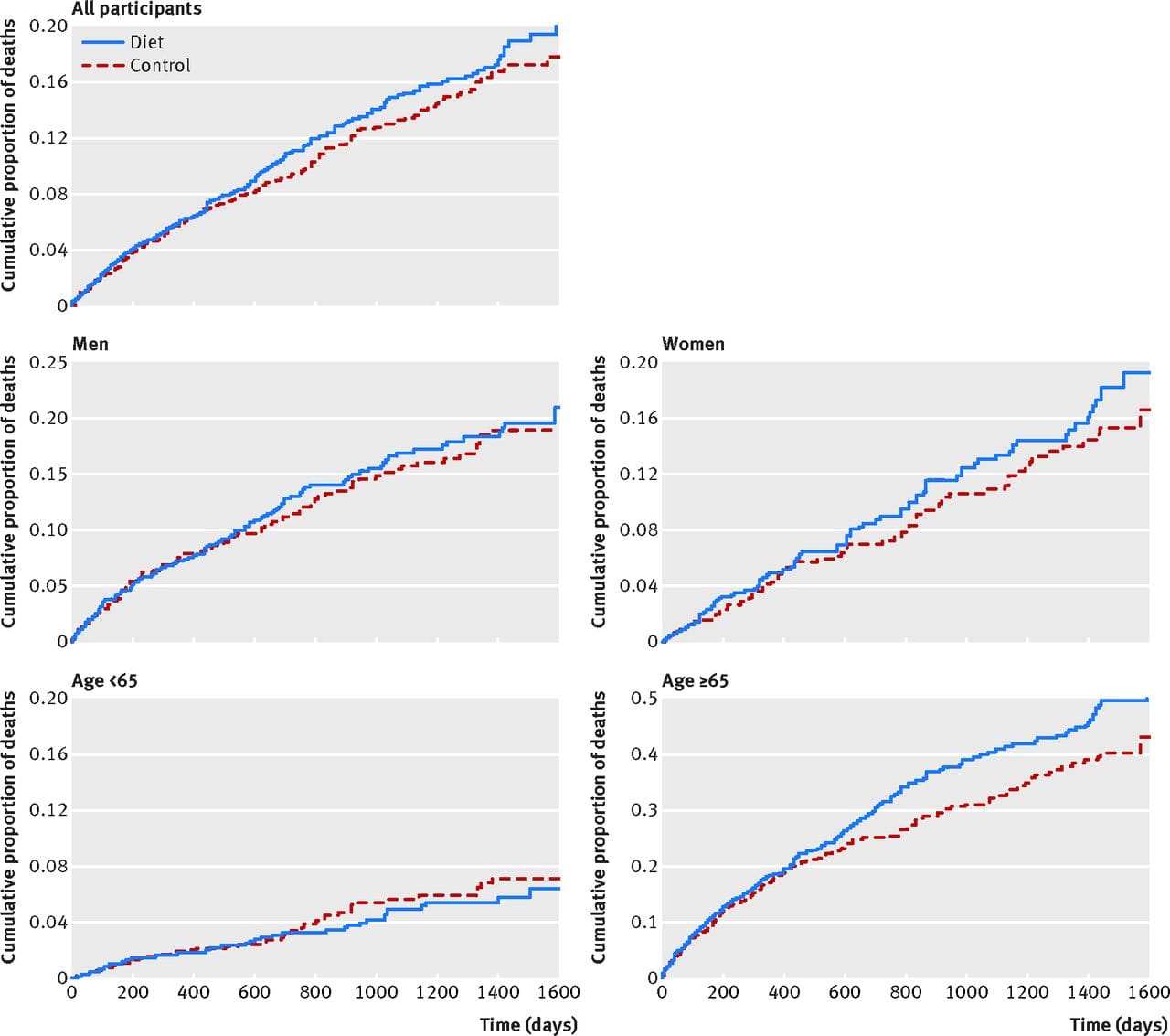
Ancel Keys first published his Seven Countries Study in 1970 which firmly established saturated fat as the enemy and the dietary-heart hypothesis as 'fact'. This study omitted data from 13 countries that didn't show the association pattern that confirmed the theory. Following this, the Minnesota Coronary Experiment showed that replacing saturated fat with unsaturated fat from vegetable oil lowered blood cholesterol but actually caused more deaths, and the results were not published in full.
The data from the original experiment has been recovered and reanalysed by Dr. Christopher Ramsden in 2016.
The experiment fed over 9,000 adults over a period of five years, either a diet with saturated fat replaced with linoleic acid (from corn oil and corn oil polyunsaturated margarine), or a control diet that was high in saturated fat from animal fats, general margarines, and shortenings.
The 2016 conclusion that wasn't published in 1973 is as follows:
"Available evidence from randomized controlled trials shows that replacement of saturated fat in the diet with linoleic acid effectively lowers serum cholesterol but does not support the hypothesis that this translates to a lower risk of death from coronary heart disease or all causes. Findings from the Minnesota Coronary Experiment add to growing evidence that incomplete publication has contributed to overestimation of the benefits of replacing saturated fat with vegetable oils rich in linoleic acid."
"There was a 22% higher risk of death for each 30 mg/dL (0.78 mmol/L) reduction in serum cholesterol."
Dr. Ramsden posits the possibility of vegetable oils increasing lipoprotein particle oxidation as contributing to an increased risk of coronary heart disease. He also makes the following note in his summary on the validity of the dietary-heart hypothesis:
"This paradigm has never been causally demonstrated in a randomized controlled trial and thus has remained uncertain for over 50 years"
The flaw in the diet-heart hypothesis is in the assumed causal mechanism; that elevated LDL cholesterol causes build up of atherosclerosic plaques. This is because LDL is one of the substances found in the plaques during autopsies. But this is like blaming the metal in bullets and guns for being the cause of death in shootings and then deciding to ban the production of steel.
LDL delivers lipids to tissues, including for repair, which partly explains why it’s found in plaques. The problem is when those particles become oxidised and trigger inflammation. It's the inflammation that is problematic, not the presence of healthy LDL.
Having lots of small, dense LDL particles (known as Pattern B) in your blood is a much better warning sign for heart disease than just looking at total LDL. These smaller particles are more easily damaged (oxidised) and slip into artery walls, where they can start the process of plaque build-up.
The problem with a standard LDL cholesterol test is that it only tells you the total amount of cholesterol inside LDL particles. It doesn’t say how many of the smaller, more harmful ones contribute to that total.
Your liver also makes VLDL particles, which carry triglycerides (fat) around the body. Having high levels of these is also strongly linked to a higher risk of heart disease.
Research shows that high triglycerides can raise your risk of cardiovascular disease by around 50-100% compared to normal levels. In contrast, total LDL cholesterol on its own is a weaker predictor - roughly a 20-30% higher risk. So tests that measure triglycerides, ApoB (a direct count of all “bad” particles) or LDL particle size and number give a much clearer picture of your true risk.
LDL cholesterol is vitally important for dozens of functions in the body. Cholesterol is needed for brain function, helping neurons send signals, and it plays a central role in hormone production, function of the immune system, and cell membrane integrity. It also allows the transport of fat-soluble vitamins (A, D, E, K) to the tissues that require it. The same pathway that produces cholesterol generates Coenzyme Q10, which is critical for mitochondrial energy production. So LDL is not “bad” - it is essential for life. The real issue is whether your LDL particles are being damaged (oxidised) or are present in excessive, small dense forms that drive plaque build-up. Rather than worrying about LDL levels we should probably be more focused on keeping our LDL healthy.