Fructose and alcohol cause metabolic syndrome
A lot of what I'm reading points the finger at fructose as a primary cause of metabolic problems such as type 2 diabetes, fatty liver and Alzheimer's disease. I've compiled some key metabolic concepts to explain what's going on with sugar.

A key thing to be aware of when trying to manage diabetes is that 'sugar' is a term applied to a range of carbohydrates. One of the things that is confusing when first starting to figure out how to manage diabetes is that the word sugar is applied to many different chemical combinations. I don't like using the term 'blood sugar' as it is inaccurate, but I still find myself habitually saying this in casual conversation. We monitor glucose levels in the blood to get a gauge of how well we're managing diabetes, but this is effectively just the canary in the coal mine, and in many ways, the 'gas' that's going to kill us is fructose... Table 'sugar' is more correctly called sucrose, and is made up of one glucose and one fructose molecule joined together. High fructose corn syrup (HFCS) has a slightly higher proportion of fructose in relation to glucose, typically 55-65% fructose.
High blood glucose levels are responsible for many complications relating to diabetes so it is important to monitor levels if you have any metabolic problems, but these high levels are largely caused by insulin resistance which is initially driven by weight gain from overconsumption of fructose and/or alcohol.
For the last two weeks, I've been listening to a new audiobook - Nature wants us to be fat by Dr. Richard J. Johnson where he goes into detail about his fructose survival hypothesis. I'm really enjoying the evolutionary history approach he's taken to investigating the causes of weight gain in humans. Our evolutionary history has taken some dramatic turns, largely due to climate changes over millions of years, that have lead us to having a fat storage pathway that, combined with the modern food system has many of us locked into a constant weight-gain mode.
How we're evolved to be excellent fat-storing animals
Dr. Johnson uses the term 'thrifty genes' to highlight the adaptations that have made us exceptionally good at storing fat and have helped our species to survive multiple mass-starvation events.
Suspected to have been an advantage following the meteor impact that wiped out the dinosaurs, dry-nosed apes (from which we are descended) lost the ability to produce their own vitamin C. This would initially seem to be a disadvantage but during times of food-shortage the resulting increase in oxidative stress placed on mitochondria causes a reduction in fat-burning and an increase in fat-storage helping animals to survive for longer periods in the event of food shortages.
Climate cooling around 10-17 million years ago is suspected to have lead to our European great ape ancestors returning to Africa, but not before they'd lost the ability to produce uricase. This genetic mutation increases our levels of uric acid after consuming fructose. Similar to the loss of vitamin C production, increased uric acid production helps to increase fat storage and reduces fat burning.
The fat storage and preservation mechanisms provided by both the lack of vitamin C and higher uric acid levels also help to provide (or generate) metabolically available water in times of drought.
The agricultural revolution began approximately 12-10,000 years ago as humans left their hunter-gatherer lifestyles behind in favour of a more controlled and predictable farming routine. An increase in the number of salivary amylase–promoting AMY1 genes in the population provides the advantage of breaking down grains and tubers more efficiently, meaning that more glucose energy can be produced from starchy foods. Interestingly, populations with a long history of starch-rich diets tend to have higher levels of AMY1 and this may be one reason why some people are more susceptible to weight gain and type 2 diabetes than others.
Insulin resistance has survival benefits
Insulin resistance is a method the body uses to ensure sufficient energy is available for the brain (which needs 20% of our daily energy resources). The brain does not need insulin to deliver glucose to the inside of most of its cells, but other organs and tissues do. So by reducing the amount of glucose delivered everywhere else, the brain can ensure high levels of glucose are available. Blocking the effectiveness of insulin is a survival tactic for an animal facing a potential shortage of food or water and is common when they hibernate or undertake a long migration. In nature, the insulin resistance resolves when the animal comes out of hibernation or reaches its destination and has lost its excess body fat. In the case of hummingbirds, they go through this cycle daily - they increase their body fat by up to 40% and their liver becomes engorged with fat while feasting on nectar during the day. Their blood glucose is extremely high by evening, reaching up to around 39mmol/L. They effectively give themselves type 2 diabetes every night and then are cured by morning due to their extremely fast metabolism (for perspective on numbers; 21mmol/L is as high as my CGM will read and I have occasionally hit that, but now I get anxious if I go above 9 and I try to stay below 7.8). The hummingbird manages to do extreme cardio in one night of sleeping that would take us months or years to clear the equivalent amount of liver-fat storage.
Leptin resistance makes you hungry
Dr Richard J. Johnson, Nature Wants us to Be Fat:
"Fructose causes leptin resistance which makes us hungrier"
Leptin is secreted by fat cells and tells the hypothalamus to signal us to stop eating. Leptin levels vary along with insulin and BMI. Fructose consumption combined with being overweight causes leptin resistance which leaves you feeling more hungry than individuals on a low fructose diet or are of a healthy weight. Being overweight also reduces the amount of fat burning and availability of energy in cells making them signal that they are still hungry so will cause habitual overeating - this is an evolutionary adaptation for animals to prepare for hibernation or migration.
Fructose metabolism
Dr Richard J. Johnson, Nature Wants us to Be Fat:
"Fructose triggers weight gain for animals in the wild."
Fructose is primarily metabolised by the liver and promotes 'de novo lipogenesis' which is the technical term for the production of fat cells from non-fat dietary sources.
Fructokinase is the enzyme responsible for the first step in fructose metabolism and is mostly concentrated in the liver. It is also present in the intestines and kidneys, and to a lesser extent in the brain. The metabolism of fructose in the liver is responsible for causing obesity and metabolic syndrome. The general driving force behind type 2 diabetes is the presence of too much fat in the liver which is caused by fructose and/or alcohol consumption.
Fructose metabolism also increases uric acid levels and triglycerides. Uric acid blunts the effects of insulin and increases blood pressure. High levels of triglycerides are a higher risk factor for cardiovascular disease than elevated LDL cholesterol. When excessivley high for long periods of time, uric acid can crystallise and cause gout.
Consistently high fructose consumption lowers basal metabolic rate (BMR) which is the rate your body uses energy when at rest, for basic bodily functions such as breathing, thinking and digesting. Fructose metabolism also promotes over-consumption of food generally due to the blocking of normal satiety hormones and the effectiveness of insulin.
Fructose has fewer checks and balances than glucose metabolism as fructokinase acts without any feedback mechanism. Cells cannot regenerate lost ATP (the body's main form of chemical energy) from the uric acid byproduct of fructose metabolism. Uric acid also causes oxidative stress on mitochondria (the energy factories within our cells) inhibiting their ability to generate ATP. Low levels of ATP in cells increase hunger to try to encourage an increase in food consumption. Continued consumption of fructose excacerbates the problem. Fructose effectively mimics starvation within cells, which flips the survival switch to the 'on' position.
The polyol pathway
We can manufacture fructose from glucose without having to consume it via the polyol pathway. This is thought to be an ancient survival mechanism, which has evolved to help us store energy and water in preparation for shortages. When the pathway is switched on, glucose is converted first into sorbitol and then into fructose. That fructose can then drive fat production, raise uric acid, and worsen insulin resistance — all things you don’t want if you’re trying to reverse type 2 diabetes.
The polyol pathway is activated by conditions that simulate stress or scarcity:
- Dehydration - triggers the body to try to conserve water, but in the process generates sorbitol which can cause cellular damage.
- A drop in blood pressure - signals reduced blood volume, again pushing the body into “survival mode.”
- High uric acid levels - both a trigger and a consequence of this pathway, creating a vicious cycle.
- Low oxygen levels (hypoxia) - limits normal energy production, so the body shifts into this alternative pathway.
Fructose as a poison
Dr Richard J. Johnson, Nature Wants us to Be Fat:
"The cause of metabolic syndrome is fructose"
I describe fructose as a "chronic poison" because you don't immediately notice the negative impact on your body as you do with alcohol (which is both a chronic and an acute poison). With alcohol, you notice getting drunk immediately (acute), whereas liver damage takes years of prolonged exposure (chronic). A common phrase in nutrition and physiology is "The dose makes the poison" (an adage from a Swiss physician called Paracelsus). My personal view is that fructose is a poison if it is consumed more frequently than we have evolved to cope with, over a prolonged period of time e.g. on a daily or weekly basis over several years. Nature has established fructose as an important substance to help us fatten up before prolonged spells of food or water shortage which is why fruits are seasonal. Our physiology has evolved to switch off our natural satiety mechanisms when supplied with fructose. This is to drive foraging and fruit-feasting behaviours to prepare us for extreme winters, failed hunts and prolonged droughts.
Dr. Robert Lustig states:
"Fructose is a poison"
This is a long 90 minute breakdown of everything you need to know about sugar and how fructose can be considered a poison. It's well worth making the time to watch this.
We've managed to invent ways to preserve and incorporate fructose into our daily diet which is preparing us for ice-age level winters that never arrive. All other animals naturally manage their weight levels with natural feedback mechanisms. These tell the animal what, when, and how much to eat e.g. birds switch from eating insects to fruit when they need to fatten up before a long migration. Lions do not count calories, but you'll never see an obese one in the wild. We were never meant to eat fructose every day in unnaturally high doses, and that is why it is making us all sick - it's a case of "The frequency, as well as the dose, makes the poison".
What to do about it
Avoiding consuming fructose is the obvious approach, but it also helps to avoid activating the polyol pathway as much as possible. We can do this by combating the activation pathways mentioned above so the following might be an ideal list of things to help keep fructose levels down:
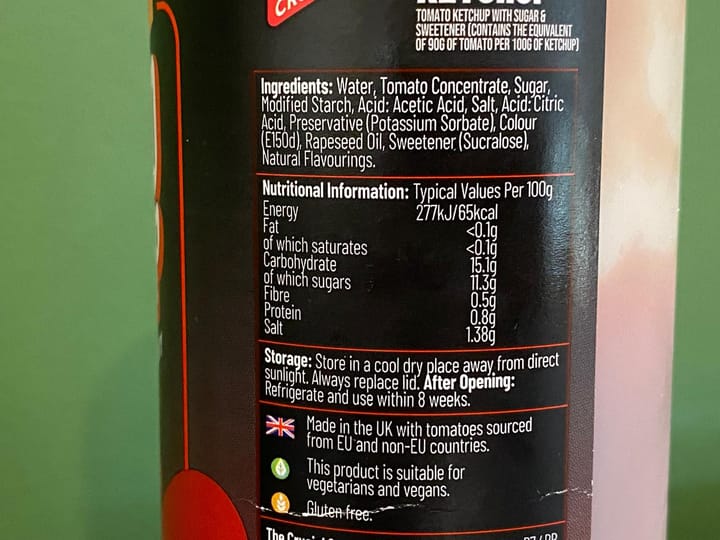
- Avoid anything with added sugar or high fructose corn syrup. In the UK it can often be called glucose-fructose syrup or isoglucose syrup. Anything ending with 'ose' is generally a sugar molecule and UPF manufacturers tend to list more than one to make it look like sugar is not the highest constituent of the food. This will also help to keep uric acid levels low and avoid activating the polyol pathway.
- Drink plenty of water (about 8 glasses per day).
- If you don't have regular access to mineral-rich water such as spring water, have a crystal or two of sea salt after drinking water (especially if you aren't eating much or are fasting). These electrolytes will help to keep your cells hydrated.
- Avoid artificial sweeteners and especially sorbitol, as it can be converted quickly into fructose.
- Reduce or avoid caffeinated and flavoured drinks as they can cause dehydration.
- Try to get plenty of vitamin C from green vegetables such as broccoli or Brussels sprouts instead of high-fructose fruits.
- Start thinking about how sugar would have played a role in fattening us up before winter as fruit becomes ripe towards the end of Summer. Remember, we wouldn't naturally have had access to it for most of the year so it makes no sense to consume it frequently. Recognise this hibernation preparation mechanism for what it is.
- If you need to lose weight try fasting or intermittent fasting to give your body a chance to experience the hibernation or famine your body has been preparing it for.
- Avoid ultra processed foods (UPF) as they are designed to be overconsumed and can block the body's normal satiety signalling mechanisms.
- Plant starches and fibre primarily contain glucose so don't worry about eating those from a fructose point of view. You may need to adjust carbohydrate totals to manage your blood glucose levels, but focus on eliminating fructose and alcohol as the underlying cause of metabolic disorder.
- Regular exercise will help to maintain stable levels of blood pressure and oxygen delivery which will help to avoid activating the polyol pathway. I always say frequency is better than intensity, so add small achievable goals to your exercise routine.
- Don't obsess about shedding all of your body fat. Having some fat available could save your life if you suddenly become ill, or there is an event which means that you don't have access to healthy food or water for a long period.
Sources
"Glucose provides “satiety” signals to the brain that fructose cannot provide because it is not transported into the brain."
"Hepatic metabolism of fructose favors de novo lipogenesis"
George A Bray et al. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity
Rats fed sucrose develop type 2 diabetes even if consuming the same amount of calories as non-sucrose fed rats who were fed starch.
"Sucrose is not simply an energy source that may have a role in obesity, but rather has specific metabolic effects that favor the development of fat accumulation and insulin resistance independent of excessive energy intake."
Carlos Roncal-Jimenez et al. Sucrose induces fatty liver and pancreatic inflammation in male breeder rats independent of excess energy intake
"Our data indicate that chronic fructose consumption induces leptin resistance prior to body weight, adiposity, serum leptin, insulin, or glucose increases..."
Alexandra Shapiro et al. Fructose-induced leptin resistance exacerbates weight gain in response to subsequent high-fat feeding
"Increased consumption of fructose for 10 weeks leads to marked changes of postprandial substrate utilization including a significant reduction of net fat oxidation. In addition, we report that resting energy expenditure is reduced compared to baseline values in subjects consuming fructose-sweetened beverages for 10 weeks."
Chad L Cox, Kimber L Stanhope et al. Consumption of fructose-sweetened beverages for 10 weeks reduces net fat oxidation and energy expenditure in overweight/obese men and women
The liver is responsible for how fructose causes obesity and metabolic syndrome. Preference for fructose is established in the intestine but metabolic issues caused by metabolism in the liver.
"Here we show that this hepatic, endogenously produced fructose causes systemic metabolic changes."
Miguel A Lanaspa et al. Endogenous fructose production and metabolism in the liver contributes to the development of metabolic syndrome