War on Diabetes Newsletter 14th June 2025

Welcome to the first War on Diabetes newsletter. Your weekly tips and ideas from someone who has had diabetes for five years and learned a lot about it. This is going to be a practical and actionable guide to things your doctor might not be telling you about.
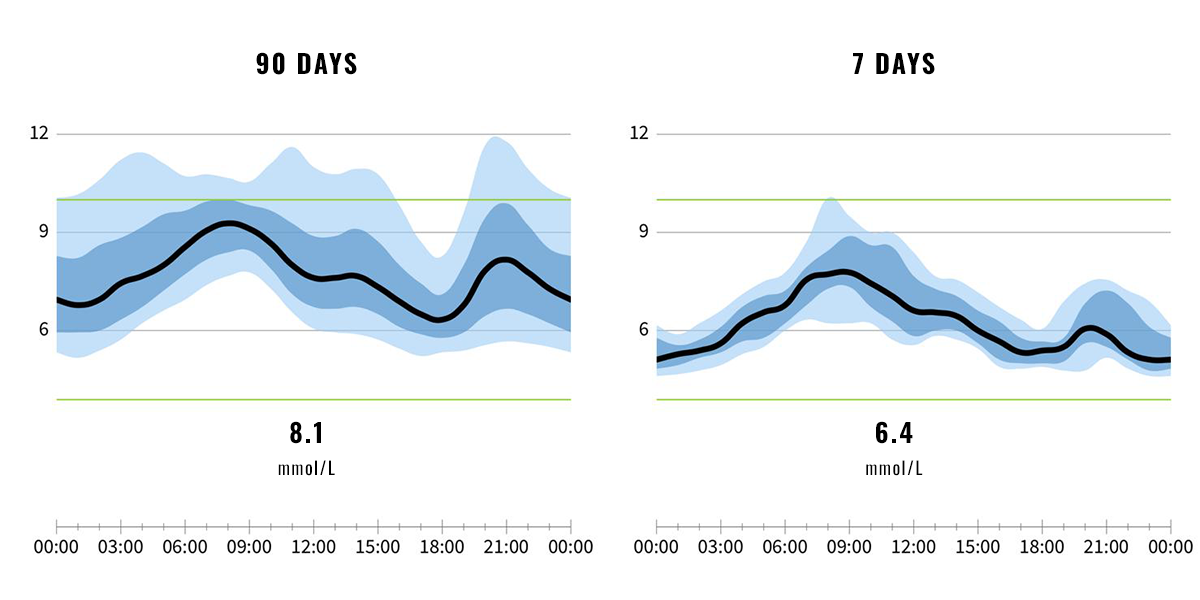
This week I've been getting more walking done and I seem to have found the right amount of daily carbs to start getting my blood sugars under control. If what I'm eating looks unachievable for you right now don't be disheartened. It's taken a lot of small steps for me to get to this point.
I've been trying out a new app called Strava and it's literally opened up a whole new world for me in discovering new walking routes. The detailed pathways on its maps mean I'm no longer held back by wondering how far a different path will take me, or how long it will take to get back. I did a 3.75 mile walk on Friday morning and normally whenever I spot a bench I usually need to sit down and stop hyperventilating for 10 minutes, but I didn't feel any need for this when I spotted this charming little guy about half way round. Don't get me wrong, I'm glad he's there for when I might need him😅
What I learned this week
Dropping my carbohydrate by 30% has drastically improved my blood glucose control in a matter of days. I also have a bit of a rant about NHS guidance implying that starches aren't fattening.
Read more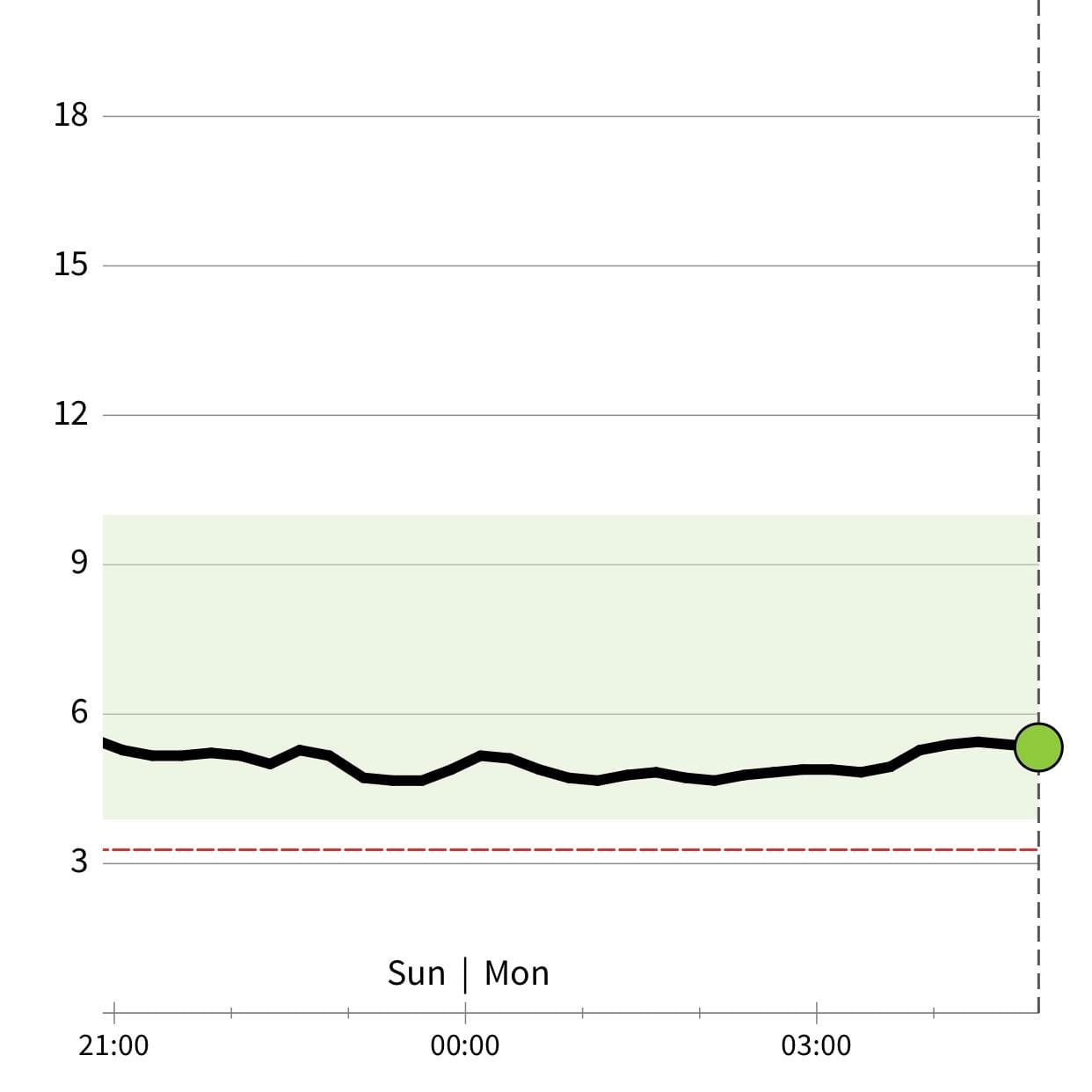
Progress Update
My first 'normal' looking overnight glucose reading. More eggs, more meat, sleeping earlier and moving more all seem to be working.
Read moreThis week's food heroes:
Itsu Chicken Noodle Soup
This is still Ultra Processed Food (UPF) which I generaly try to avoid, but this is a good compromise for blood glucose control if you're at the office and need something quick. Glass noodles seem to have minimal impact on levels compared to rice or wheat noodles. I suspect it's because they're made from mung beans instead. Adding the optional egg is good for protein and fat which keeps you full for the afternoon.

Chicken Soup-Broth with Salad
I don't generally like liquidising food but adding a bit to bone broth is a fair exception and this soup was made with the remains of a chicken used for a Sunday roast dinner: just boil it for a couple of hours and add some left over vegetables (e.g. leeks, onions, carrots etc) and blend it up and pop in the fridge for when you need something easy later in the week. You can add left over cooked chicken to it when you warm it up. I like to add some chopped green beans or other green veggies to up the fiber a bit. For salad, I wash it all in one go and wrap in foil or put in tupperware after a food shop or when I first use it so then I can just grab handfulls of it for lunches and brightening up dinners when I can't be bothered cooking any green veg. Adding a dash of apple cider vinegar to salad is a quick way to add flavour and helps to keep glucose spikes down amongst many other health benefits.

Pork and Bacon Linguine with Sugar Snaps in Cream Sauce
I've found linguine or spaghetti to be one of the less-impactful carbs for blood glucose control. I have about half to a quarter of what I'd consider a normal portion (or at least what I used to eat). I find having carbs at the end of a meal helps to make it more satisfying as you finish it and if you leave eating them towards the end of a meal, the fiber, fat and protein help to dampen the resulting glucose spike. I've included this one because was my dinner the evening before I dropped 0.5 mmol/L on my 7-day average glucose (it's normally a mission to drop 0.1).


What I learned last week
"Oh dear..." - Caffeine vs dawn effect. My morning cuppa gets the boot.
Read moreNew Recruit Tip
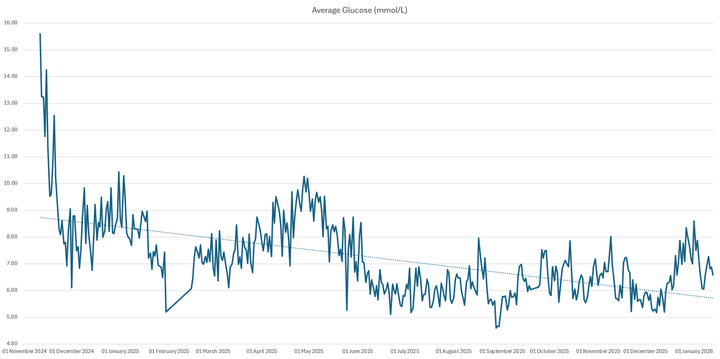
If you've recently been diagnosed with type 2 diabetes or pre-diabetes then it's worth trying a Continuos Glucose Meter (CGM). Your healthcare advisor probably won't like this idea because it's considered as only necessary for type 1 diabetes and they'll be worried about prescription costs. CGMs are expensive at around £60 and they only last two weeks but the information you can get even in that short time frame will guide you as to how your body is responding to different foods. It's been the key to me figuring out how to get down from a HbA1c of 133 to 48 mmol/mol (14.3% - 6.5%). I couldn't have done it without the information from my CGM. It's not like a hyperdermic injection, its a flexible tip that sits just under your skin and doesn't hurt. If you've been recently diagnosed, it's worth being aware of the fact that it is much easier to get type 2 diabetes into remission now than in several years, or decades later. The sooner you get on top of it, the easier it will be.
Get a free FreeStyle Libre 2 PlusDiabetes Veterans
Have you ever met my old friend, 'denial'? I've found denial sets in when progress stalls and you're not sure why, or you might know why but you just fall into a habit of putting off changes until tomorrow, the weekend or after an upcoming event that has been stressfull in planning. I've been there for three long stretches of time in five years. Greggs for lunch, drinking cider and other bad habits... With type 2 diabetes it's the thought process of, "High blood glucose isn't going to kill me this week, so I've got time later to sort it out." Having a six month gap between HbA1c tests and disheartening morning finger prick tests were my downfall. If only someone had told me about the dawn effect and how stupid it is to try to measure fasting glucose first thing in a morning, I might have defeated denial a lot sooner. This week's tip, if you're doing finger prick tests then do them just before you have your evening meal or get a CGM before you need one for measuring insulin doses. Once you go on inulin injections for type 2 diabetes, you're driving the underlying cause of hyperinsulinemia. I can't really speak for type 1 diabetes but did you know they are ten times more likely to suffer from cardiovascular diesease than metabolically healthy individuals? For type 2 diabetics, the risk is six times - which is suprisingly a lot less. I suspect that's because with type 1, injecting insulin solves the problem of high blood sugar in the short term, so for them denial could be "I can eat whatever I want as I can just inject more insulin." and that may be driving hyperinsulinemia even further. Another habit I've recently heard about for type 1s is that some of them deliberately underdose their insulin in order to keep weight off so that would have the opposite problem of keeping the body stuck in fat-burning mode.
Recommended reading - Jason Fung "The Diabetes Code"